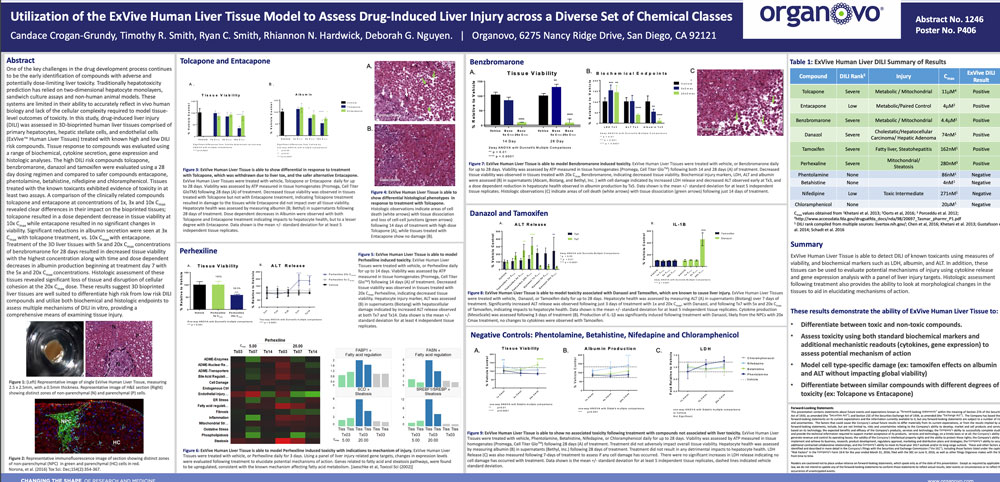
Utilization of the ExVive human liver tissue model to assess drug-induced liver injury across a diverse set of chemical classes
Publication Summary:
One of the key challenges in the drug development process continues to be the early identification of compounds with adverse and potentially dose-limiting liver toxicity. Traditionally hepatotoxicity prediction has relied on two-dimensional hepatocyte monolayers, sandwich culture assays and non-human animal models. These systems are limited in their ability to accurately reflect in vivo human biology and lack of the cellular complexity required to model tissue level outcomes of toxicity. In this study, drug-induced liver injury (DILI) was assessed in 3D-bioprinted human liver tissues comprised of primary hepatocytes, hepatic stellate cells, and endothelial cells (ExVive™ Human Liver Tissues) treated with known high and low DILI risk compounds. Tissue response to compounds was evaluated using a range of biochemical, cytokine secretion, gene expression and histologic analyses. The high DILI risk compounds tolcapone, benzbromarone, danazol and tamoxifen were evaluated using a 28 day dosing regimen and compared to safer compounds entacapone, phentolamine, betahistine, nifedipine and chloramphenicol. Tissues treated with the known toxicants exhibited evidence of toxicity in at least two assays. A comparison of the clinically related compounds tolcapone and entacapone at concentrations of 1x, 3x and 10x Cmax revealed clear differences in their impact on the bioprinted tissues; tolcapone resulted in a dose dependent decrease in tissue viability at 10x Cmax while entacapone resulted in no significant changes in viability. Significant reductions in albumin secretion were seen at 3x Cmax with tolcapone treatment, vs. 10x Cmax with entacapone. Treatment of the 3D liver tissues with 5x and 20x Cmax concentrations of benzbromarone for 28 days resulted in decreased tissue viability with the highest concentration along with time and dose dependent decreases in albumin production beginning at treatment day 7 with the 5x and 20x Cmax concentrations. Histologic assessment of these tissues revealed significant loss of tissue and disruption of cellular cohesion at the 20x Cmax dose. These results suggest 3D bioprinted liver tissues are well suited to differentiate high risk from low risk DILI compounds and utilize both biochemical and histologic endpoints to assess multiple mechanisms of DILI in vitro, providing a comprehensive means of examining tissue injury.
View Publication