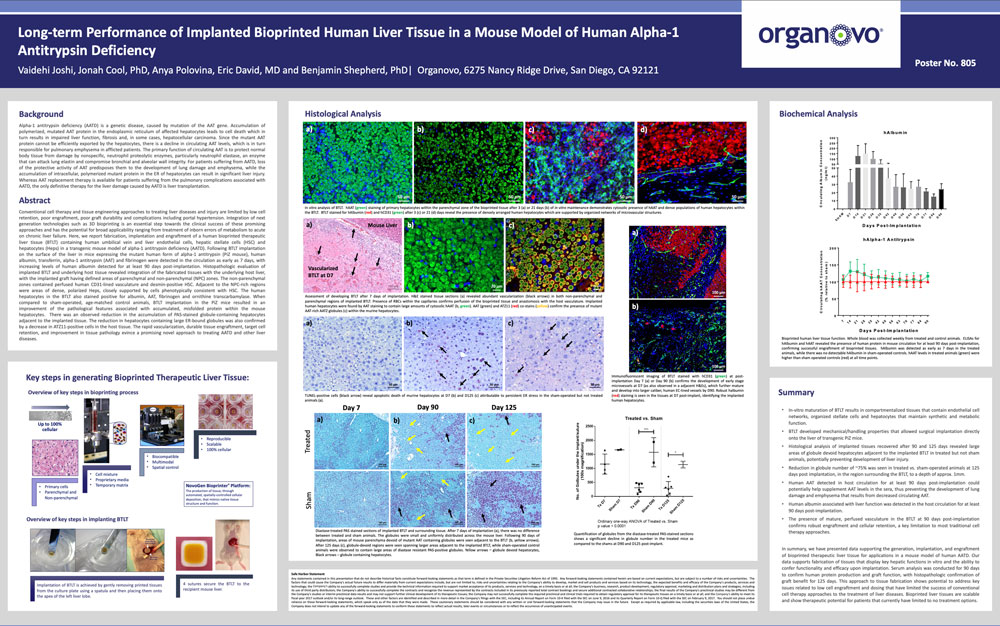
Long-term performance of implanted bioprinted human liver tissue in a mouse model of human alpha-1 antitrypsin deficiency
Publication Summary:
Conventional cell therapy and tissue engineering approaches to treating liver diseases and injury are limited by low cell retention, poor engraftment, poor graft durability and complications including portal hypertension. Integration of next generation technologies such as 3D bioprinting is an essential step towards the clinical success of these promising approaches and has the potential for broad applicability ranging from treatment of inborn errors of metabolism to acute on chronic liver failure. Here, we report fabrication, implantation and engraftment of a human bioprinted therapeutic liver tissue (BTLT) containing human umbilical vein and liver endothelial cells, hepatic stellate cells (HSC) and hepatocytes (Heps) in a transgenic mouse model of alpha-1 antitrypsin deficiency (AATD). Following BTLT implantation on the surface of the liver in mice expressing the mutant human form of alpha-1 antitrypsin (PiZ mouse), human albumin, transferrin, alpha-1 antitrypsin (AAT) and fibrinogen were detected in the circulation as early as 7 days, with increasing levels of human albumin detected for at least 90 days post-implantation. Histopathologic evaluation of implanted BTLT and underlying host tissue revealed integration of the fabricated tissues with the underlying host liver, with the implanted graft having defined areas of parenchymal and non-parenchymal (NPC) zones. The non-parenchymal zones contained perfused human CD31-lined vasculature and desmin-positive HSC. Adjacent to the NPC-rich regions were areas of dense, polarized Heps, closely supported by cells phenotypically consistent with HSC. The human hepatocytes in the BTLT also stained positive for albumin, AAT, fibrinogen and ornithine transcarbamylase. When compared to sham-operated, age-matched control animals, BTLT implantation in the PiZ mice resulted in an improvement of the pathological features associated with accumulated, misfolded protein within the mouse hepatocytes. There was an observed reduction in the accumulation of PAS-stained globule-containing hepatocytes adjacent to the implanted tissue. The reduction in hepatocytes containing large ER-bound globules was also confirmed by a decrease in ATZ11-positive cells in the host tissue. The rapid vascularization, durable tissue engraftment, target cell retention, and improvement in tissue pathology evince a promising novel approach to treating AATD and other liver diseases.
View Publication